- Home
- Common Foot Problems
- Shin Splints
Medial Tibial Stress Syndrome
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

Medial tibial stress syndrome (MTSS) is a common overuse injury resulting in pain and tenderness along the lower shin bone.
More commonly known as "Shin Splints", MTSS typically affects runners, but is also a common problem for athletes, dancers and military personnel.
With MTSS, repetitive overuse of the muscles that attach to the shin irritates the underlying bone, resulting in inflammation and tenderness.
Here we will look at the common causes, symptoms and diagnosis of medial tibial stress syndrome, and then go on to look at the best shin splints treatment and prevention options.
What Are Shin Splints?
Medial Tibial Stress Syndrome is defined as a stress reaction to the tibia that is typically caused by overuse.
There are a couple of different things that are thought to occur around the shin bone with shin splints:
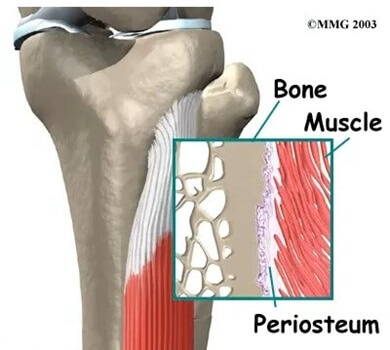
- Inflammation: The outer surface of the shin bone is covered by a membrane known as the periosteum. There are a number of muscles that attach to the shin bone e.g. soleus & tibialis posterior, and as they contract, they pull on the periosteum. If there is excessive traction through the muscles, this can irritate the periosteum resulting in localised inflammation, known as periostitis or periostalgia
- Bone Stress: repetitive overloading of the shin bone can cause increased stress and force through the bone. This can lead to micro-damage and increased remodelling as the bone tries to heal itself which can lead to pain
Medial Tibial Stress Syndrome Causes
There are a number of factors that can lead to shin splints, and some of the most common medial tibial stress syndrome causes are:
- Overuse and Repetitive Stress: The most common cause of medial tibial stress syndrome is overuse and repetitive stress on the tibia and connected muscles. Engaging in high-impact activities, such as running, jumping, dancing, or playing sports that involve frequent stopping and starting, can lead to micro-trauma in the tibia, periostitis, resulting in shin splints.
- Rapid Changes in Activity: Quickly increasing the intensity, duration, or frequency of physical activity without allowing the body time to adapt is another common cause of shin splints. This abrupt change can overwhelm the muscles and bones, leading to injury – they need time to adapt to new stress levels. This is particularly common in people who are returning to sport after an injury, or individuals with previously low activity levels.
- Poor Biomechanics: Biomechanical issues related to how your body moves and functions can play a significant role in the development of medial tibial stress syndrome. Some common factors include:
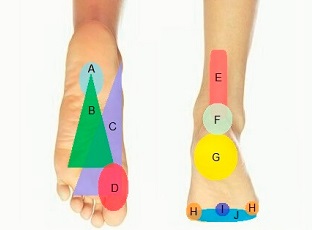
Pronation: Overpronation (excessive inward rolling of the foot) can contribute to MTSS, as it increases the stress on the medial (inner) aspect of the shin.
Flat Feet: People with flat feet may experience altered shock absorption, leading to increased strain through the tibia. It can also affect muscle activity which places further stress through the periosteum, leading to periostitis
Gait Abnormalities: Irregularities in your walking or running gait can lead to uneven distribution of forces, increasing the risk of shin splints.
- Inadequate Footwear: Wearing shoes that lack proper cushioning, support, or stability can increase the risk of medial tibial stress syndrome. Everyone’s feet are slightly different and will benefit from different footwear/support – more on that later!
- Hard Training Surfaces: Training on hard or uneven surfaces, such as concrete or uneven terrain, can amplify the impact on your lower legs, contributing to the development of medial tibial stress syndrome.
- Muscle Imbalance: Imbalances in the muscles surrounding the shin can also be a contributing factor with MTSS. Weakness, tightness and fatigue in certain muscle groups, particularly tibialis posterior (responsible for controlling foot inversion) and the calf muscles, can lead to increased stress on the tibia during physical activity.
- Lack of Proper Warm-up and Stretching: Skipping warm-up routines and neglecting to stretch properly before exercise can make the muscles and tendons more susceptible to injury. A lack of flexibility in the calf muscles can increase the risk of medial tibial stress syndrome.
- Gender Differences: Females may be more susceptible to medial tibial stress syndrome due to variations in things such as lower limb alignment, bone density and hormonal factors.
- Proximal Control: Proximal control, aka core strength, refers to the ability to stabilize the core and pelvis while performing lower extremity (leg and foot) movements. Poor proximal control can lead to altered lower limb mechanics, increasing the risk of shin splints.
- Previous Shin Splints: If you have had medial tibial stress syndrome in the past, you are at increased risk of developing it again, particularly if the underlying causes where not fully addressed
- Vitamin D Deficiency: some studies have shown a link between vitamin D deficiency and an increased risk of developing MTSS
It's important to note that these medial tibial stress syndrome causes can often overlap and vary from person to person. Many individuals may have a combination of these risk factors. Medial tibial stress syndrome most frequently affects runners, dancers and military recruits.
MTSS Symptoms
Medial tibial stress syndrome is typically characterized by a range of symptoms that can vary in severity which typically manifest along the inner edge of the shin bone. Common shin splints symptoms include:
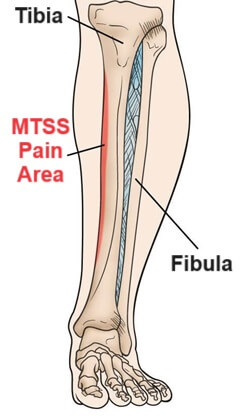
- Shin Pain: The most common and prominent medial tibial stress syndrome symptom is pain. It usually presents as a dull, aching pain along the inner aspect of the shin which may be quite intense at times, and some people experience a sharp, razor-like pain. MTSS pain usually extends down the lower two-thirds of the medial tibial border (the inner side of the shin).
- Tenderness: With medial tibial stress syndrome, the affected area is usually tender to the touch. Pressing or applying any pressure on the inner edge of the shin bone usually elicits discomfort and tenderness, typically extending over an area of at least 5cm.
- Pain During Activity: MTSS pain often begins or worsens during physical activities that involve weight-bearing on the legs e.g. running or jumping, particularly when the feet hit the ground. In the early stages of shin splints, the pain may actually improve after initial activity e.g. a few minutes into a run, but as the condition worsens, symptoms may get progressively worse and stop you from being able to complete your exercise session.
- Pain After Activity: After physical activity, medial tibial stress syndrome pain may persist, sometimes intensifying in the hours following exercise or the next day. This delayed onset of pain is a common hallmark of more chronic MTSS but usually settles within 48 hours. Pain from shin splints doesn’t usually affect your sleep.
It's important to note that the severity of these symptoms can vary from person to person. Some individuals may experience mild discomfort that doesn't significantly interfere with their activities, while others may have more intense pain that affects their ability to participate in physical activities.
Shin Splints Diagnosis
Diagnosing medial tibial stress syndrome typically involves a combination of clinical evaluation and, in some cases, diagnostic imaging:
1. History
Your healthcare provider, often a sports medicine specialist or physical therapist, will start by discussing your medical history and current symptoms. They will want to know about your physical activities, exercise routines, previous injuries and medical conditions. They will ask you about your current symptoms including pain location, nature and severity of your pain, functional limitations and symptom progression
2. Examination
They will carry out a comprehensive physical examination, particularly focussing on muscle strength, flexibility, biomechanics, foot position and your walking pattern. They will also palpate (apply gentle pressure) to the affected area to assess for tenderness. Pain on resisted plantarflexion (where you point your feet down at the ankles against resistance) indicates likely MTSS.
3. Imaging
While medial tibial stress syndrome can usually be diagnosed from your history and physical assessment, your healthcare provider may send you for further imaging to confirm the diagnosis and rule out other possibilities:
- X-rays: are usually normal with shin splints but may be used to look for stress fractures in the shin bone
- MRI: are more sensitive showing soft tissue as well as bone, and will usually show periostitis if there is medial tibial stress syndrome
- CT: high-resolution CT scans are also an option but they are less sensitive than an MRI for diagnosing shin splints
Differential Diagnosis
There are a few other conditions that can present in a similar way to medial tibial stress syndrome but with subtle differences:
- Stress Fracture: pain when running but localised tenderness is over a smaller area of around 1-2cm. Tibial stress fracture are usually visible on x-ray as a black line
- Nerve Entrapment: nerve damage is also accompanied by tingling, numbness and loss of sensation in the lower shin
- Exertional Compartment Syndrome: bilateral symptoms (both legs affected), gets worse with exercise and settles quickly with rest (usually within 30 minutes). It is also associated with loss of local pulses, tingling or numbness, pallor and the skin may feel cold to touch
- Tendinopathy: inflammation or degeneration of one of the lower limb tendons e.g. Achilles tendonitis can cause similar pain to medial tibial stress syndrome, but in a slightly different location
- Popliteal Artery Entrapment: where the blood flow to the lower leg is compromised will also cause changes in skin colour, cramping, numbness and a feeling of heaviness in the legs
Medial Tibial Stress Syndrome Treatment
The treatment of medial tibial stress syndrome typically involves a combination of strategies aimed at reducing pain, promoting healing, and preventing recurrence. Here's a comprehensive overview of the best treatment options for shin splints:
1. Rest and Activity Modification
Rest is a fundamental component of medial tibial stress syndrome treatment. It allows the body time to heal and reduces stress on the affected area. Activities that exacerbate symptoms, such as running or high-impact sports, should be temporarily avoided, usually for around 2-6 weeks.
Activity modification may involve switching to lower-impact exercises during the healing phase, such as swimming or cycling, to maintain cardiovascular fitness without aggravating the condition.
2. Ice Treatment
Applying ice to the affected area can help reduce pain and inflammation from medial tibial stress syndrome. Ice should be applied for 15-20 minutes at a time, several times a day. Always wrap ice in a towel – don’t place it directly on the skin.
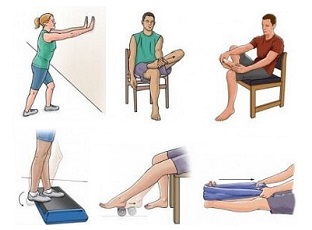
3. Medial Tibial Stress Syndrome Exercises
Rehabilitation exercises play a significant role in the treatment of medial tibial stress syndrome. These exercises are designed to improve lower leg strength, flexibility, and stability. A physical therapist can provide a tailored exercise program based on your specific needs and progress which may involve:
Shin Splints Stretches
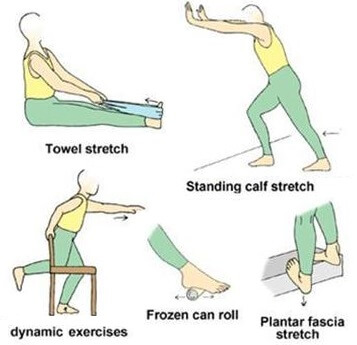
Stretches are an important part of MTSS treatment and usually target the calf muscles and shin muscles, as well as any other tight leg muscles:
- Calf Stretches: targeting both gastrocnemius and soleus
- Quads Stretches: for all four quads
- Hamstring Stretches: for the muscles on the back of the thigh
- Glute Stretches: for the buttocks
- Foot & Ankle Stretches: for the muscles controlling foot movements
MTSS Strengthening Exercises
Strengthening exercises for medial tibial stress syndrome help to improve the strength, stability and endurance of the lower limb muscles. Strengthening exercises for shin splints usually include:
- Calf Strengthening: e.g. heel raises
- Quads Strengthening: e.g. squats
- Hamstring Strengthening: e.g. bridging
- Glute Strengthening: e.g. the clam
- Balance & Proprioception Exercises: to improve stability around the shin and foot position
- Core Stability Exercises: to improve body position and proximal control e.g. Pilates, help improve overall body mechanics during physical activity
4. Orthotics For Shin Splints

Custom or over-the-counter orthotic insoles can help provide better arch support and correct any biomechanical issues, such as overpronation, that may contribute to medial tibial stress syndrome. A physical therapist or orthotist will be able to advice you on the best style for you depending on your foot shape and position.
5. Footwear
Ensuring that you have appropriate footwear for your activity is essential. Your shoes should provide adequate:
- Cushioning: especially in the heel and midsole areas to absorb impact and reduce the stress on the tibia
- Stability: shoes with a stable platform and reinforced heel counters can help control foot motion and maintain proper alignment
- Support: shoes with proper arch support are essential as they help maintain the foot’s normal alignment and prevent overpronation
Consider the type of physical activity you engage in and choose shoes designed for that specific activity. Running shoes, for example, are designed to accommodate the repetitive impact of running, while cross-training shoes are suitable for various activities.
And remember, athletic shoes have a limited lifespan as the cushioning and support can degrade over time. It's recommended to replace your athletic shoes regularly, usually every 300-500 miles for running shoes or every 6-12 months, depending on use.
6. Gait Analysis
Gait analysis, carried out by a podiatrist or physical therapist, can identify any irregularities in your walking or running pattern, allowing for more targeted treatment and recommendations.
7. Shin Splints Medication
Medication for shin splints, such as over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) e.g. ibuprofen, can be used to manage pain and reduce inflammation. However, their use should be supervised by a healthcare professional.
8. Shin Splints Massage
Massage can you a useful tool when treating medial tibial stress syndrome. Massage for shin splints typically targets tight calf muscles to release any tension, tightness or trigger points. It is important however to avoid massaging the affected area of the shin else that can make things worse!
9. Gradual Return to Activity
Once the pain has subsided and strength and flexibility have improved, a gradual return to normal activities can begin. Starting with low-impact exercises and slowly increasing intensity and duration is crucial to prevent a recurrence of symptoms.
How To Avoid Shin Splints
There are a number of things you can do when it comes to preventing medial tibial stress syndrome or to reduce the risk of recurrence:
- Proper Warm-up: Always warm up before exercise with dynamic stretches and gentle movements
- Strengthen Muscles: Building strength in your calf muscles and tibialis posterior can help reduce the risk of MTSS
- Gradual Progression: When starting a new exercise routine or increasing the intensity of your activities, do so gradually to allow your body to adapt
- Footwear and Orthotics: Invest in quality, supportive footwear designed for your specific activity. Orthotic inserts can also help correct biomechanical issues
- Cross-Training: Incorporate a variety of activities into your fitness routine to reduce the repetitive stress on your legs
- Training Surface: Where possible, train on soft surfaces such as grass or astroturf, rather than concrete to reduce the stress on your shins.
MTTS Summary
What Are Shin Splints? Medial tibial stress syndrome is an overuse injury that causes inflammation and irritation along the inner border of the lower shin
What Causes Shin Splints? Overuse and repetitive stress on the lower leg, especially during activities like running or jumping, muscle imbalance, poor biomechanics and inadequate footwear
Common Symptoms Of Shin Splints? Dull, aching pain and tenderness along the inner edge of the lower two thirds of the shin that gets worse with activity
How To Treat Shin Splints? Shin splints are treated with rest, RICE protocol (Rest, Ice, Compression, Elevation), rehabilitation exercises, proper footwear, and by addressing any underlying biomechanical issues
Do Shin Splints Go Away? With appropriate treatment and rest, shin splints typically improve and can go away, allowing individuals to return to their regular activities. You may need to rest from aggravating activities for 2-6 weeks and it can take 3-6 months to make a full recovery from medial tibial stress syndrome
Shin Splints Vs Stress Fracture? Shin splints and stress fractures both cause shin pain, but they differ in nature. Shin splints result from overuse and involve inflammation of soft tissues, while stress fractures are actual tiny fractures in the bone due to repetitive stress, often requiring more extensive recovery and potentially immobilization.
How To Prevent Shin Splints? Preventing medial tibial stress syndrome involves gradual progression of activity, proper footwear selection, strength and flexibility exercises, and biomechanical assessment, as well as listening to your body and recognizing early signs to avoid overuse injuries.
Page Last Updated: 9th January, 2026
Next Review Due: 9th January, 2028