- Home
- Common Foot Problems
- Tendonitis Guide
- Posterior Tibial Tendonitis
Posterior Tibial Tendonitis
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board
Posterior tibial tendonitis is a common cause of inner foot pain and inflammation.
If you get pain or swelling on the inner side of your ankle, are finding it difficult to stand on tiptoes or have noticed your foot arch starting to drop, chances are posterior tibial tendonitis is to blame.
The posterior tibial tendon is the main stabiliser of the lower leg and plays a crucial role in supporting the main foot arch and preventing the foot from rolling over.
When caught early, posterior tibial tendonitis is fairly easy to treat. But, without proper diagnosis and treatment, it gradually progresses through four different stages, which can result in permanent foot deformity.
It is also known as Tibialis Posterior Tendon Dysfunction, Tibialis Posterior Insufficiency or Acquired Adult Flat Foot (AAFF) and is one of the most common causes of inner foot pain.
What Is Posterior Tibial Tendonitis?
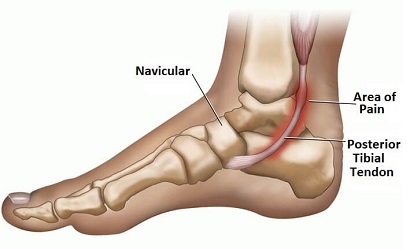
With posterior tibial tendonitis there is inflammation, degeneration or tearing in the tibialis posterior tendon of the foot.
The posterior tibial tendon is extremely important as it supports and controls the medial foot arch. It is the thick cord-like structure that connects the posterior tibial muscle, aka tibialis posterior, found on the back of the shin underneath the calf muscles, to the inner side of the foot on the navicular bone.
The tibialis posterior tendon passes close to the Achilles tendon in the lower calf and then hooks round underneath the prominent inner ankle bone, the medial malleolus.
This area, at the bottom of the shin bone, is the most common place for problems to develop in the tendon as the blood supply here is poor.
This means the tendon doesn’t receive the oxygen and nutrients required to keep it healthy or to repair from any damage.
Once the tendon is damaged or inflamed, the medial foot arch will gradually collapse resulting in a flat foot.
What Causes Posterior Tibial Tendonitis?
Posterior tibial tendonitis is usually caused by:
- Injury: Ankle sprain, fracture or direct blow to the inner ankle which damages the posterior tibial tendon
- Overuse: high-impact sports e.g. football or basketball, or running or hiking may damage the tibialis posterior tendon due to repetitive use and over-loading
- Demographics: Typically affects people over the age of 40, and is more prevalent in women than men
- Altered Foot Biomechanics: People who already have flat feet are more prone to developing posterior tibial tendonitis as it places more force through the tendon
- Footwear: Whilst not a specific cause, wearing shoes that do not provide adequate foot arch support can be a contributing factor
- Accessory Navicular: approximately 10% of the people have a small extra piece of bone, an accessory navicular, that sits within the posterior tibial tendon and can cause irritation
- Obesity: Being overweight places extra strain on the posterior tibial tendon making it prone to injury
- Inflammatory Arthritis: Certain medical conditions such as rheumatoid arthritis and gout increase the risk of developing tendonitis
Posterior Tibial Tendonitis Symptoms
Typical symptoms of posterior tibial tendonitis include:
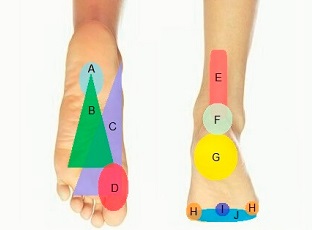
- Pain & Swelling: Pain and inflammation from posterior tibial tendon injuries commonly causes foot arch pain that tends to be felt around and behind the inner ankle region and down the side of the foot into the in-step. If the nearby nerve is affected you may also get a burning, stabbing or shooting nerve pain and tingling into the foot.
- Unable To Stand On Tiptoes: The most classic sign of posterior tibial tendonitis is difficulty standing up on your tiptoes. It may be painful as you push-up onto your tiptoes (known as a heel raise) or you may be completely unable to rise-up at all.
- Reduced Mobility: People suffering from posterior tibial tendon dysfunction are often limited in how far they can walk. There is typically an achy pain on the inner side of the foot and ankle as soon as you start walking which gets progressively worse the longer you are on your feet, making long distances impossible. Standing for long periods is often increasingly painful and running may be impossible.
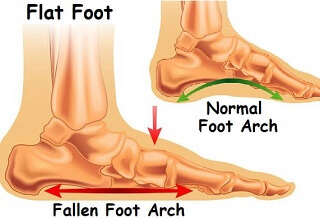
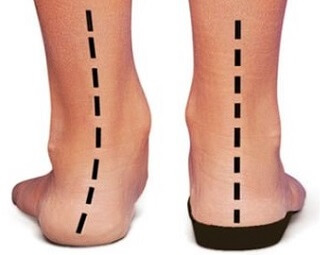
- Flat Foot Deformity: A gradual loss in height of the medial foot arch is common with tibialis posterior tendinopathy.
As the tendon weakens it is unable to support the foot and the foot flattens completely which alters the position of the foot bones. - Stiffness: Ankle movement is often limited, particularly lifting the foot upwards (dorsiflexion). This is usually due to tightness in the calf muscles.
Stages & Progression
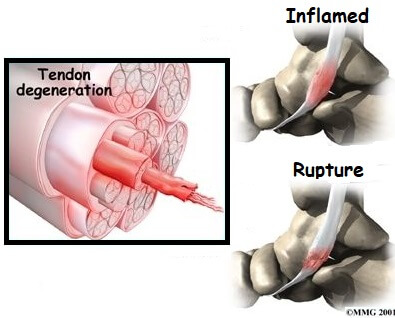
Without treatment, posterior tibial tendonitis tends to get worse and worse. Prolonged stretching, inflammation and subsequent degeneration of the tibialis posterior tendon not only weakens the tendon but puts it at risk of tearing.
Left untreated, Posterior Tibial Tendon Dysfunction progresses through four different stages:
- Stage 1: Minor tendon damage and inflammation due to overstretching. Mild pain and swelling along the tendon. Medial ankle pain when walking. No foot deformity
- Stage 2: Partial tearing of the tendon. Increasing ankle and foot pain, swelling and flattening of the foot. Unable to stand on tiptoes on the affected foot
- Stage 3: Further tearing of the tendon. Complete loss of the medial foot arch. Heel becomes “fixed”, known as rigid flatfoot deformity, which is difficult to correct
- Stage 4: Complete rupture of the tendon. Permanent deformity of the foot and adjacent ankle joint.
Posterior Tibialis Tendonitis is much easier to treat in the early stages. Once it has progressed to or beyond stage 2, surgery is often required.
#CommissionEarned from Amazon on qualifying purchases
Non-Operative Treatment
Treatment for stage 1 posterior tibial tendonitis usually involves a combination of:
- Rest: Avoid activities that bring on your symptoms as much as possible. Try and stick to activities that don’t place much force through the foot such as swimming and cycling. In more severe cases, your doctor may recommend crutches
- Ice: Regularly applying ice packs 3-4 times a day for around 10 minutes to the inner ankle helps to reduce pain and inflammation. You can get specially designed ankle ice wraps that strap to the ankle so they stay in place perfectly rather than slipping off when you move. To find out how to use ice safely and effectively, visit the ice treatment section
- Compression: Wearing a tubigrip compression bandage helps to reduce swelling and support the ankle. It should be worn double thickness from the mid-foot to just below the knee, during the day only.
- Elevation: Whenever you are resting, try and keep your leg elevated, preferably so your ankle is higher than your chest, to reduce any swelling. Make sure the knee is supported. Leg Elevation Cushions tends to work better than a standard pillow or cushion as they are a better size and hold their shape well.
- Medication: Taking pain-relieving medication e.g. paracetamol/acetaminophen and anti-inflammatories (NSAIDs) e.g. ibuprofen/Advil regularly can help to reduce the pain and inflammation – always check with your doctor before starting on medication
- Gels/Creams: Rubbing certain creams or gels into the affected area of the foot can really help to reduce pain and inflammation from posterior tibial tendonitis. Tiger Balm and Arnica are two of the most popular choices and can make a big difference
- Orthotics: There are a whole range of orthotics that can be helpful with posterior tibial tendonitis.
Shoe inserts help to correct foot position by supporting the medial arch and heel.
Custom-made ankle supports, braces or AFO’s (ankle function orthoses) help to improve the stability of the ankle and foot and reduce the tension and force through the tendon - Footwear: It is important to wear supportive shoes. Ideally you want flat, sturdy lace-up shoes that have enough space to incorporate your orthotics. Try and wear your shoes and orthotics whenever you are walking, even around the house – avoid going bare-foot as much as possible
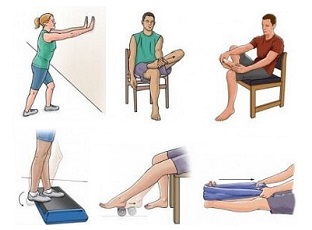
- Physiotherapy: You will be given a rehab plan involving ankle strengthening exercises and calf stretches to improve the strength and mobility of the posterior tibial tendon and the surrounding muscles. These will again help to improve the support and flexibility around the ankle, reducing the tension through the tibialis posterior tendon
- Ankle Immobilisation: Your doctor may advise wearing a cast or removable boot for 1-2 months with posterior tibial tendonitis. These hold the ankle and foot in a fixed position and reduce the tension on the tendon to allow it time to heal
- Steroid Injection: Corticosteroid injections are sometimes used to reduce pain and inflammation in tendons, but they are rarely advisable with posterior tibialis tendinopathy as there is a high risk of the tendon rupturing.
All of these treatments are most effective during the first stage of posterior tibial tendonitis.
Surgical Treatment
If non-surgical posterior tibial tendonitis treatment has failed, meaning there has been no benefit over 6 months, and you are stage 2 or higher, then you are likely to need surgery. In some cases, ankle immobilisation may be sufficient during stage 2, but this is rare.
Surgery for posterior tibial tendonitis aims to reduce pain, improve function and reduce the progression of posterior tibial tendon dysfunction.
The type of surgery carried out will depend on how much tendon damage there is and which part of the tendon is affected. Surgery for tibialis posterior dysfunction may involve one of more of the following:
- Debridement: Any inflamed parts of the posterior tibial tendon tissue are removed. This is only effective in the early stages of posterior tibial tendonitis before the foot has changed shape
- Achilles Lengthening: If the Achilles tendon is particularly tight, it is released to allow greater ankle movement and reduce the tension on tibialis posterior
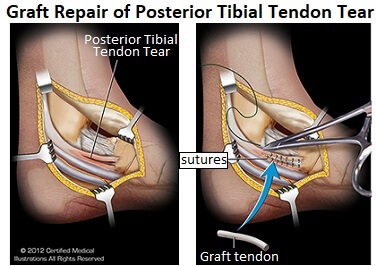
- Tendon Transfer: This is where the damaged portion of the tibialis posterior tendon is removed and replaced with one of the other foot or ankle tendons.
Typically surgeons will use part of the tendon of:
Flexor Digitorum Longus: which helps bend the outer four toes down
Flexor Hallucis Longus: which bends the big toe downwards
Tibialis Anterior: which pulls the foot upwards. This is known as a Cobb Procedure
People can typically walk normally after the tendon transfer procedure, but they may have difficulty running and may not be able to resume certain sports. - Osteotomy: This is where one or more of the foot bones are cut and their position shifted and fixed, most typically the heel bone, to recreate a “normal” foot position. The bones are fixed into place using plates or screws and are sometimes removed once the bones have healed
- Fusion: Sometimes an osteotomy is sufficient to correct the foot position, in which case the bones in the back of foot are fused. The cartilage between the foot bones is removed and the bones are held together with plates and/or screws. Over time, the individual bones gradually fuse together to become one bone. The foot will still be able to move up and down but sideways movement is lost.
Patients who require surgery for their posterior tibial tendonitis, particularly osteotomies or fusions generally have very limited ankle and foot movement, moderate to severe pain, and are very limited in how far they can walk prior to surgery. While surgery may seem extreme for posterior tibial tendonitis, people typically find they have much less pain and can actually walk better after surgery.
Recovering From Surgery

You are usually discharged home a day or two after surgery for posterior tibialis tendonitis. If you have had a tendon transfer or osteotomy, you will most likely have a plaster cast to hold your foot in the correct position (slightly turned inwards) to allow the foot to heal.
A physiotherapist will teach you how to walk, get up and down stairs and in and out of a car using a frame or crutches. Typically, you are not allowed to put any weight through the operated foot for a number of weeks.
If you have a cast, it is usually replaced every 2 weeks gradually bringing the foot to a neutral position at which point you can start taking your weight through the foot again – this often takes 6 weeks. You may need to continue using a cast for a number of weeks, after which time, you will be given a removable boot to wear.
Most people are walking normally within 3 months of posterior tibial tendonitis surgery. Low-impact sports can be resumed after 6 months but it may take a year before you can return to all activities.
You will have regular physiotherapy to improve your strength and flexibility and you may need to wear orthotics in your shoes to ensure a good foot position.
Most people make a good recovery after surgery for posterior tibial tendon dysfunction and are walking normally within 3 months of their operation. You can usually return to work after around 4 weeks, but it may be longer if you have a manual job. Low-impact sports can be resumed after 6 months but it may take a year before you can return to all activities.
Possible Complications
Every operation has potential complications. The most typical risks of posterior tibial tendonitis surgery are:
- Ongoing Pain: The pain not be completely relieved although it should be better than it was before surgery. If the plates and screws are causing pain then your surgeon may be able to remove the metalwork provided the bone has healed
- Non-Union: This is where the bones fail to unite (stick together) with an osteotomy or fusion
- Infection: The wound may become infected, which would typically be treated with antibiotics. Infection is a rare complication with any type of surgery
- Swelling: Some swelling initially is normal, but if it increases or persists, you should see your doctor
- Blood Clot: All surgery carries a risk of blood clots but DVT’s (deep vein thrombosis) and PE’s (pulmonary embolus) are rare
- Numbness or Tingling: You may notice some ongoing numbness or pins and needles around the surgical site. This is because some of the nerves are cut or stretched during surgery to access the bones and tendons. It normally settles down after a few months, but there may be some ongoing sensory changes that never fully resolve
Posterior Tibial Tendonitis Summary
Posterior tibial tendonitis is a common cause of inner foot pain and weakness.
Inflammation and degeneration in the posterior tibial tendon result in pain and swelling around the inner foot arch.
Posterior tibial tendonitis symptoms often include difficulty standing on tiptoes, flat foot deformity, ankle stiffness and difficulty walking
Common causes of tibialis posterior tendonitis include ankle injuries, repetitive overuse, altered foot biomechanics, obesity and inflammatory conditions.
Treatment depends on the severity of the tendonitis but may include a combination of rest, ice, elevation, medication, orthotics and steroid injections.
Exercises are a key part of the recovery process, whatever stage of posterior tibial tendonitis you have. Strengthening exercises for the foot and ankle muscles and calf stretches all help to reduce the tension and force through the tendon.
There are a number of other conditions that cause pain in the same area as posterior tibial tendonitis so if this isn't sounding quite like your problem, visit the inner foot pain diagnosis sections or find out about the other types of foot tendonitis.
You may also be interested in the following articles:
- Pain On Top Of Foot
- Outer Foot Pain
- Pain On Bottom Of Foot
- Heel Pain
- Nerve Pain In The Foot
- Swollen Feet & Ankles
- Foot Numbness
- Foot Lumps & Bumps
Related Articles
Page Last Updated: 4th February, 2026
Next Review Due: 4th February, 2028