- Home
- Common Foot Problems
- Tarsal Coalition
Tarsal Coalition
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

Tarsal Coalition is a problem in the foot that causes pain and stiffness, typically starting during adolescence.
With tarsal coalition, some of the bones in the foot or ankle fuse together or become abnormally connected, creating a rigid and inflexible area.
Also known as tarsal synostosis, it is typically a congenital problem i.e. something you are born but can be caused by a foot injury or infection.
Tarsal Coalition is one of the rarer causes of side of foot pain affecting approximately 1 in every 100 people. One or both feet may be affected.
Symptoms of tarsal coalition often come on very suddenly resulting in side foot pain, fatigue and foot cramps often causing people to walk abnormally. It can cause other foot problems such as ankle sprains and abnormal foot biomechanics. Tarsal coalition treatment usually consists of surgery, shoe inserts or casting to immobilise the foot.
What Is Tarsal Coalition?
The bones at the back of the foot are known as the tarsal bones, made up of the talus, calcaneus, cuboid, navicular and cunieform bones.
Tarsal coalition is a condition where two of the tarsal bones become become attached to each other by abnormal growth of either:
- Bone: Osseus Coalition (synostosis)
- Cartilage: Cartilagenous Coalition (synchondrosis)
- Fibrous Tissues: Fibrous Coalition (syndesmosis)
This abnormal growth forms a "bridge" or "bar" between the two bones. The extent of the join varies from mild to extensive.
The most common types of tarsal coalition are:
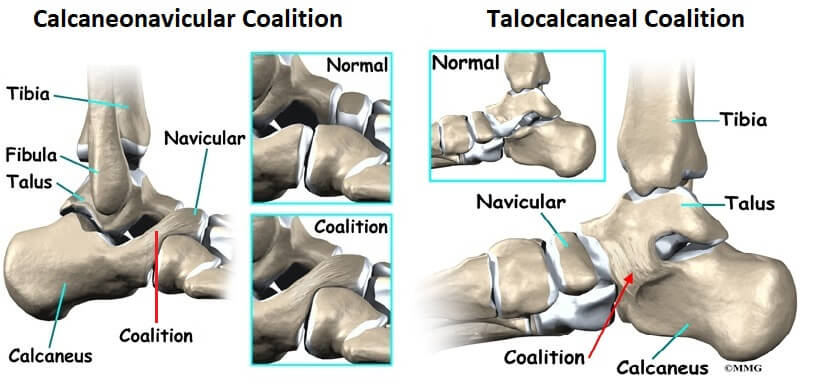
- Calcaneonavicular Coalition: between the calcaneus (heel bone) and the navicular aka CN bar
- Talocalcaneal Coalition: between the calcaneus and the talus aka TC bar
These account for over 80% of cases of tarsal coalition but bridges can form between other tarsal bones.
Tarsal coalition restricts the normal movement between the two bones resulting in stiffness and immobility in the hind/mid foot region. This in time impacts on the surrounding joints and can lead to degenerative arthritis.
What Causes Tarsal Coalition?
There are a number of things that can cause tarsal coalition:
- Genetic Abnormality
- Foot Trauma
- Infection
- Arthritis
Let's find out a little more about each of these.
1. Genetic Abnormalities
Most cases of tarsal coalition are congenital due to a genetic mutation which affects how the individual tarsal bones develop.
A process called mesenchymal segmentation fails to happen properly so rather than developing as separate structures, two or three of the tarsal bones become connected.
There is thought to be a genetic link with tarsal coalition and in some cases, it may be associated with genetic disorders such as Ehlers-Danlos syndrome or Marfan syndrome.
2. Foot & Ankle Injuries
Foot injuries can also cause tarsal coalition. Injuries, such as fractures or sprains, can disrupt the normal development of the connective tissue between the bones of the foot or ankle. This can lead to abnormal growth of this tissue (known as synostosis), which can cause the bones to fuse together or become abnormally connected.
3. Infections
Infection can increase the risk of developing tarsal coalition. Certain illnesses can weaken the bones and soft tissue in the foot, causing them to become abnormally connected.
Additionally, infections caused by bacterial and fungal organisms can lead to inflammation, which can disrupt the normal development of connective tissue and lead to synostosis.
4. Arthritis
Arthritis can increase the risk of developing tarsal coalition. Certain types of arthritis, such as rheumatoid arthritis, can cause joint inflammation and degeneration of the bones and soft tissues in the foot, making them more prone to abnormal growth and fusion.
Certain medications used to treat arthritis have also been associated with the development of tarsal coalition. Therefore, it is important to monitor your condition if you have arthritis or are taking medications to manage it.
Tarsal Coalition Symptoms
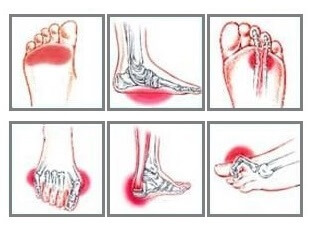
Typical symptoms of tarsal coalition include:
- Foot & Ankle Stiffness: and rigidity in the back of the foot, known as the hindfoot
- Foot Pain: below the ankle and at the back of the foot, worse when weightbearing or with activity e.g. standing, walking, running
- Flat Foot Arches: reduced height of foot arches in one or both feet
- Muscle Spasms: increased spasticity in the peroneal muscles causing calf pain
- Limping: when walking, particularly long distances

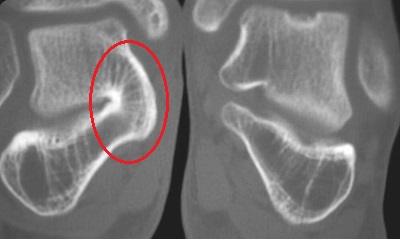
Symptoms of tarsal coalition don't usually appear until a child reaches around 10 years of age as that is when their bones start to mature.
Up until this point, much of the foot structure is soft cartilage which gradually changes and hardens, through a process called ossification, to bone. If there is a coalition structure present, it will ossify too.
This ossification happens at different ages depending on which bones are involved:
- Calcaneonavicular Coalition: typcially ages 8-12 years
- Talocalcaneal Coalition: typically ages 12-15 years
Prior to ossification, people don't usually develop any symptoms of tarsal coalition. But once the area starts to harden it may start to cause problems and heel pain may develop.
Only around one quarter of people who have tarsal coalition will get symptoms from it, in most cases it goes completely unnoticed. Many only experience symptoms in adulthood or if they develop secondary conditions such as arthritis or suffer from a foot injury.
How Is Tarsal Coalition Treated?
Tarsal coalition only requires treatment if it is causing symptoms, otherwise it is best left alone. Many symptomatic cases can be treated non-operatively but in just over 50%, surgery may be required.
Non-Operative Treatment
Non-operative treatment for tarsal coalition includes:
- Rest: Avoiding aggravating activities for 4-6 weeks reduces the stress on the tarsal bones and can reduce pain
- Shoe Inserts: Orthotics e.g. heel wedges or arch supports can be used to correct abnormal foot position, stabilize the foot and reduce the forces going through the affected joint
- Temporary Immobilization: with a below knee cast/boot and crutches for 6 weeks to take the weight and stress off the tarsal bones - abolishes symptoms in around 30% of people
- Injections: A mixture of anesthetic and steroid can be injected into the area to reduce pain, inflammation and spasming
- Medications: Non-steroidal anti-inflammatories such as ibuprofen can help to reduce the pain and inflammation associated with tarsal coalition
- Physical Therapy: gentle range of motion exercises, calf stretches, massage and ultrasound
These treatments help to reduce the symptoms of tarsal coalition but do not correct the deformity.
Tarsal Coalition Surgery
Tarsal coalition surgery is indicated if:
- Symptoms have failed to settle with non-operative treatment
- Coalition involves more than 50% of the joint surface
Surgery will depend on the location and severity of the tarsal coalition, the condition of the surrounding joints and the age and activity level of the person. The two options are:
- Resection: Removal of the coalition to restore normal movement. The coalition bridge is surgically removed and replaced with muscle or tendon and fatty tissue.For calcaneonavicular coalition they use part of the extensor digitorum brevis muscle and for talocalcaneal coalition they use part of the flexor hallucis longus tendon. Foot deformities can also be corrected at the same time.
- Arthrodesis: The affected joint is fused so the bones are held in the correct position by screws, pins or a screw-and-plate system. This prevents any movement at the joint and is typically done for larger coalitions or when there are associated degenerative changes.
Following each type of tarsal coalition surgery, you are normally given a cast or boot to immobilise the foot, and crutches as you will not be allowed to take weight through the foot for a few weeks while it heals. After this, you will start physical therapy in order to regain mobility and strength in your foot.
It can take 6-12 months to fully recovery from tarsal coalition surgery, but surgery is successful in around 85% of cases.
Tarsal Coalition Recovery
Most people make a full recovery from tarsal coalition with the right treatment. The goal of treatment is to reduce inflammation, improve flexibility, and offload pressure on the affected area.
Tarsal coalition can last for weeks, months, or even years, depending on the severity of your condition. If the symptoms are mild, conservative treatments like rest, physical therapy, and the use of braces or orthotics may be enough to reduce the discomfort and improve flexibility. In more severe cases, however, surgery may be necessary to excise the abnormal tissue.
Differential Diagnosis
Tarsal coalition is just one possible cause of ankle and heel pain.
There are a number of other conditions that can cause similar symptoms to tarsal coalition.
Flat feet can cause pain and swelling, while heel spurs and plantar fasciitis can lead to pain in the heel and arch of the foot. Tarsal tunnel syndrome occurs when an inflamed nerve gets compressed due to a structure in the foot.
Peripheral neuropathy is a condition caused by nerve damage and can lead to burning, tingling, or numbness.
You may also be interested in the following articles:
- Pain On Top Of Foot
- Foot Arch Pain
- Foot & Ankle Stretches
- Swollen Feet & Ankles
- Foot Numbness
- Burning Foot Pain
- Foot Lumps & Bumps
Summary
Tarsal coalition is a congenital foot problem that can cause pain and stiffness in the foot due to a bridge forming between two tarsal bones. It is present in around 1% of the population but does not always cause any problems.
Treatment usually involves a combination of rest, orthotics, injections and medications but the more severe cases may require tarsal coalition surgery.
Most people make a good recovery from tarsal coalition with the correct treatment.
Tarsal coalition is just one possible cause of foot pain - for help working out what is wrong visit the foot pain diagnosis section.
Related Articles
References
1. Joints Journal: Talonavicular Coalition as a Cause of Foot Pain. By A. Macera, F. Teodonno, C. Carulli, A. Borrego and M. Innocenti
2. Science Direct: Tarsal Coalition. By M.Myerson MD & A. Kadakia MD. 2019
3. Resection of Tarsal Coalition. Southampton Children's Hospital. March 2019
Page Last Updated: 19th November, 2024
Next Review Due: 19th November, 2026