- Home
- Common Foot Problems
- Heel Pad Syndrome
Heel Pad Syndrome
Written By: Chloe Wilson BSc(Hons) Physiotherapy
Reviewed By: FPE Medical Review Board

Heel pad syndrome is a common, but often overlooked cause of deep, bruise-like central heel pain.
It happens when the fat pad loses its cushioning and no longer absorbs shock properly.
Treatment focuses on cushioning, rest, supportive footwear, taping and targeted exercises.
Heel pad syndrome often gets mistaken for plantar fasciitis but the two conditions are totally different and need very different treatment approaches.
In this article, we will look at what heel fat pad syndrome is, what it feels like, what causes it, how we diagnose it, and most importantly, how to heal it and stop it coming back again.
What Is Heel Fat Pad Syndrome?
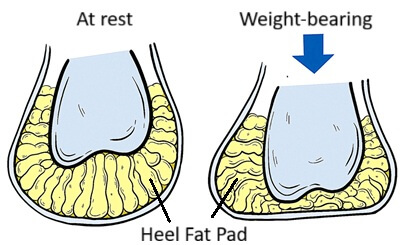
Heel pad syndrome is where there is thinning or irritation of the special heel cushion.
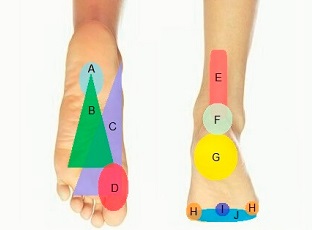
Your heel has a thick pad made up of specialized fatty tissue that sits within a honeycomb-like structure of strong, fibrous and elastic connective tissue.
The heel fat pad acts like a shock-absorbing cushion every time your foot hits the ground. It protects the heel bone (calcaneus) and helps evenly distribute pressure during walking, running, and standing.
Heel fat pad syndrome occurs when this fat pad becomes:
- Thinner (fat pad atrophy)
- Inflamed or irritated
- Less effective at absorbing shock
When this cushioning breaks down, impact forces transfer directly into the heel bone, causing deep, central heel pain.
Heel pad syndrome may also be referred to as fat pad atrophy, heel fat pad syndrome, heel fat pad atrophy or fat pad syndrome.
What Does Heel Pad Syndrome Feel Like?
Common symptoms of fat pad syndrome include:
- Deep, central heel pain or bruise-like pain directly under the heel bone
- Pain with direct pressure to the middle of the heel
- Pain that worsens when walking barefoot or on hard floors
- Aching pain that gets worse the longer you are on your feet
- Pain during high-impact activities e.g. running or jumping
- Slight relief when walking on soft, cushioned surfaces or when wearing cushioned shoes
If you feel like you are “walking on a stone,” that is classic Heel Pad Syndrome.
Unlike plantar fasciitis, heel fat pad pain doesn’t usually hurt first thing in the morning or radiate to the foot arch.
What Causes Heel Pad Atrophy?
Heel fat pad syndrome usually develops when the natural cushioning under your heel becomes overloaded, inflamed, or simply wears out. Common causes of fat pad pain include:
- Overuse or High-Impact Activities: Repetitive running, jumping, and long periods of standing, especially on hard surfaces e.g volleyball, tennis, running, basketball, dance and gymnastics.
- Age-Related Fat Pad Atrophy: As we age, the fat pad slowly becomes thinner and less springy due to a natural decline in collagen and tissue elasticity.
- Foot Mechanics: Certain foot shapes, such as flat feet or high arches, can change the way force is distributed through the heel, overstressing the fat pad. Your walking pattern e.g. how your foot strikes the ground can cause the heel pad to wear down over time.
- Inappropriate Footwear: Wearing shoes with thin or hard soles, poor cushioning and little arch support increases the impact travelling through the heel.
- Injury: A direct blow to the heel, such as landing hard on the heel when falling from a height, can trigger inflammation in the fat pad.
- Being Overweight: Extra body weight increases the load on the heel, speeding up fat pad wear and tear.
- Other Medical Conditions: Some medical conditions can increase the risk of developing heel fat pad syndrome, such as diabetes, rheumatoid arthritis and lupus.
Diagnosing Heel Pad Pain
Heel pad syndrome is typically diagnosed through a combination of clinical assessment and in some occasions imaging studies.
A foot specialist or physical therapist will check:
- The exact location of your heel pad pain
- Whether pain increases when pressing directly on the middle of the heel
- For pain when squeezing the heel from both sides (positive heel squeeze test)
- Pain patterns on soft vs hard surfaces
- Your footwear, gait, and foot mechanics
Whilst not always necessary, you may be sent for imaging studies:
- Ultrasound or MRI can show thinning or disruption of the heel fat pad
- X-rays rule out fractures or bone conditions
Diagnosis of heel fat pad syndrome is mostly clinical, but imaging is useful for persistent or unclear cases.
Conditions to Rule Out
Not all heel pain is caused by heel pad syndrome, so it is important to rule out other conditions with similar symptoms. Here are the main conditions to consider:
1. Plantar Fasciitis
- Typically causes sharp pain at the inner edge of the heel, especially with the first steps in the morning
- Pain may radiate along the arch, unlike the central bruised pain of heel fat pad syndrome
Find Out More: Plantar Fasciitis
2. Calcaneal Stress
Fracture
- A small fracture in the heel bone can mimic deep heel pad pain.
- Often associated with sudden onset pain, swelling, and tenderness that worsens with weight-bearing.
Find Out More: Foot Stress Fractures
3. Baxter’s Nerve Entrapment
- Compression of the lateral plantar nerve can cause heel pain, burning, or tingling.
- Usually more nerve-related symptoms than fat pad syndrome.
4. Retrocalcaneal Bursitis
- Inflammation of the bursa at the back of the heel.
- Pain is located at the back of the heel, rather than the central underside.
Find Out More: Heel Bursitis
Tip: A clear understanding of pain location, timing, and activity triggers usually distinguishes heel pad syndrome from other conditions, but a professional assessment is always recommended if symptoms persist.
#CommissionEarned from Amazon on qualifying purchases
How To Heal Heel Fat Pad Syndrome
Heel pad pain responds extremely well to structured treatment, especially when started early.
Below are the key evidence-based treatments for pain in the heel pad that we recommend.
1. Cushioning & Protection
This is the number one heel pad pain treatment. Your goal is to recreate the shock absorption your heel pad has lost.
- Use deep heel cup insoles (silicone or gel works best) and cushioned socks to provide extra cushioning for the heel
- Choose cushioned trainers with good support over hard-soled shoes
- Avoid barefoot walking on hard floors
2. Reduce Impact Forces
Reducing the forces going through the heel fat pad temporarily is another vital part of heel pad pain treatment.
- Stay off your feet as much as possible and avoid running, jumping or high-impact exercise. Instead swap to cycling or swimming.
- Reduce standing and walking time on hard surfaces
- Swap hard floors for carpeted areas when possible
- For rigid or high-arched feet, cushioned insoles help redistribute force.
3. Fat Pad Taping Heel

Heel fat pad taping helps pull the heel tissue back under the bone, improving cushioning and reducing pain.
Strips are applied around the heel to centralise the fat pad and support impact absorption.
Check out this helpful video from Peak Form Health Center showing how to do heel fat pad taping.
4. Ice
Apply an ice pack to the heel for 10–15 minutes after activity to reduce pain and inflammation as part of your daily heel pad pain treatment.
5. Physical Therapy
A physical therapist can provide a
- Tailored Rehab Program: strengthening and stretching exercises
- Gait Retraining: shortening your stride, encouraging mid-foot loading and improving hip and knee alignment can significantly reduce heel pressure
- Manual Therapy: such as soft tissue work and joint mobilisations to combat any tightness or stiffness and improve foot mechanics
In severe fat pad atrophy, specialist treatment options include gel injections and fat grafting. These are less common heel pad syndrome treatments but may help where the fat pad has significantly thinned.
As a physical therapist who has treated many cases of heel fat pad atrophy, I find early cushioning and load modification make the biggest difference.
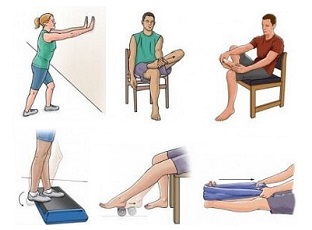
Heel Pad Syndrome Exercises
Heel pad syndrome exercises can really help to reduce heel pad pain. While they won’t “regrow” the fat pad, they can really improve load distribution, stability, and shock absorption
a) Calf Stretch
Calf stretches help to reduce excessive heel loading during walking.
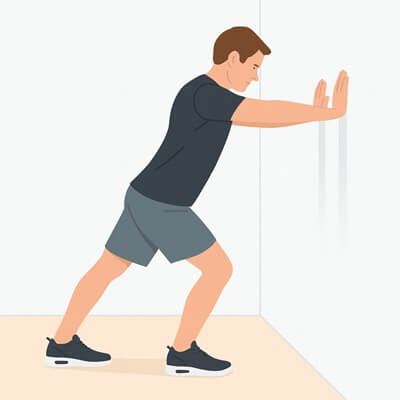
How to do it:
- Stand facing a wall
- Step one foot back
- Keep heel down
- Lean forward until you feel a stretch in your calf for 30 seconds
- Repeat 3–4 times
Find out more about Calf Stretches
b) Toe Flexor Strengthening
Strengthening the intrinsic foot muscles helps support heel mechanics.

How to do it:
- Place a towel on the floor
- Scrunch it toward you using your toes
- Repeat for 1–2 minutes
Find Out More in the Exercises For Heel Pain Section
c) Foot Arch Control Exercise
This helps improves foot stability, reducing the pressure on the heel fat pad.

How to do it:
- Sit or stand barefoot
- Gently lift your foot arch without curling your toes
- Hold 10 seconds
- Repeat 10–15 times
Find Out More in the Exercises For Heel Pain section.
d) Glute Med & Hip Stability Work

Whilst it may seem strange to focus on the glutes and hip muscles for foot pain, strengthening these muscles really helps to improve foot and knee biomechanics which helps reduce the impact through the heel when walking.
There are various different exercises that can help such as Side-lying leg lifts, Monster walks and Single-leg balance drills.
Visit the glute strengthening exercises section on our sister site to find a whole range of exercises that can help reduce heel pad pain.
Recovery & Prognosis
Most people start noticing improvement within 2–6 weeks of starting these heel fat pad treatments, especially once cushioning and footwear changes are made.
Full recovery from fat pad pain usually takes 6–12 weeks, depending on:
- Severity of fat pad atrophy
- How quickly you adjust your activities
- Whether biomechanical issues are addressed
Chronic heel pad pain can be slower (18+ weeks), but still responds very well to unloading, cushioned insoles, and strengthening.
Ignoring fat pad pain symptoms or continuing high-impact activity can significantly delay healing.
How To Prevent Heel Fat Pad Syndrome
To stop heel pad irritation from returning:
- Wear supportive, cushioned, shock-absorbing footwear
- Replace worn-out shoes frequently
- Avoid walking barefoot on hard surfaces
- Use heel cups if you stand for long periods
- Strengthen your intrinsic foot and calf muscles
- Maintain a healthy bodyweight
- Gradually increase activity levels — avoid sudden spikes
Long-term protection from heel pad atrophy is all about reducing impact through the heel.
FAQs
1. What Is The Difference Between Heel Pad Syndrome & Plantar Fasciitis?
1. What Is The Difference Between Heel Pad Syndrome & Plantar Fasciitis?
Heel pad syndrome causes deep, central heel pain that feels like a bruise or a sore spot directly under the heel bone. The pain gets worse on hard floors, prolonged standing, or walking, and often improves with cushioning or heel cups.
Plantar fasciitis, on the other hand, causes sharp or stabbing pain on the inner side of the heel and foot arch pain, especially with the first steps in the morning or after sitting. The pain is linked to irritation of the plantar fascia, the thick band of tissue along the bottom of the foot.
2. Can I Still Walk With Heel Fat Pad Syndrome?
2. Can I Still Walk With Heel Fat Pad Syndrome?
Yes, you can usually walk with heel fat pad pain, but hard surfaces and long periods on your feet often make the pain worse. Cushioning and heel cups can make walking more comfortable.
3. Does A Fat Pad Go Away?
3. Does A Fat Pad Go Away?
Once the fat pad thins, it doesn’t fully grow back, but symptoms can significantly improve with proper cushioning, footwear, taping, and heel exercises to reduce impact on the heel.
4. When Should I See A Doctor For Heel Pad Pain?
4. When Should I See A Doctor For Heel Pad Pain?
See a doctor if the pain in the heel pad is severe, persistent for more than 2–3 weeks, linked to an injury, causing swelling or bruising, or not improving with rest and cushioning.
5. How Common Is Heel Fat Pad Atrophy?
5. How Common Is Heel Fat Pad Atrophy?
Pain in the heel pad becomes more common with age and high-impact activity. It frequently occurs in runners, people who stand for long periods, and adults over 50.
Fat Pad Syndrome Summary
Heel pad syndrome is a common but often overlooked cause of deep, central heel pain. It is often misdiagnosed as plantar fasciitis.
Fat pad syndrome occurs when the heel’s shock-absorbing fat pad becomes irritated, thins out, or loses cushioning.
Common causes include ageing, repetitive impact, high-impact sports, hard surfaces, poor footwear, and gait imbalances that increase pressure on the heel.
Heel fat pad atrophy typically feels like a deep, central, bruised pain that worsens with walking or standing on hard floors and improves on soft or cushioned surfaces.
The best heel fat pad syndrome treatments focus on reducing heel impact with cushioned shoes, heel cups, taping, physical therapy and heel exercises to support the foot and lower leg.
Most people recover well from heel pad syndrome in a few weeks with the right approach, and preventing recurrence is usually as simple as wearing cushioned shoes, avoiding hard surfaces barefoot, and keeping foot muscles strong.
You may also be interested in the following article
Related Articles
Page Last Updated: 27th November, 2025
Next Review Due: 27th November, 2027